- About Us
About RSIS International
Publication Method
Conference
Contact Us
- Journals
- Conference Proceedings
Days
Hours
Minutes
Seconds
Submission Deadline
Factors Influencing Coping Mechanisms in Seeking Primary Health Care Services in the Child-Headed Households in Kagera Region, Tanzania.
Khalid Peter Mwakabwale
Institute of Development Studies, University of Dar es Salaam
Dr. Florian Silangwa*
University of Dar es Salaam, Institute of Development Studies,
Child-headed households (CHHs) are a relatively new household structure that has emerged due to an increased number of orphans resulting from the death of one or both parents due to pandemics, wars, and natural disasters. Despite the Primary Health Care (PHC) waiver and exemption policy in Tanzania, accessing PHC services among CHHs has been challenging.
The study assessed factors influencing coping mechanisms in CHHs seeking primary health care services. It was characterised by a convergent parallel mixed method design in data collection, analysis, and interpretation, employing both quantitative and qualitative methods. Four hundred thirty CHHs from Muleba and Bukoba districts were sampled for household interviews, with 16 Focus Group Discussions and 22 Key Informants Interviewers.
The study found that, despite CHHs residing closer to the PHC facilities, the majority never visited the facilities despite falling sick; among those who attended, the majority paid for the services. Additionally, the majority of CHH respondents are not aware of the existence of the exemption and waiver policy. Those who did not visit the facilities applied two primary coping mechanisms whenever they got sick. The use of personal unprescribed herbal medicines, and others reported visiting traditional healers.
Lack of knowledge about the availability of PHC exemption and waiver policy for vulnerable populations, lack of money to pay, and hostility toward health workers are primary factors that limit CHHs’ access to PHC services, hence influencing the adaptation of other coping mechanisms to mitigate health problems.
KeyWords: Child Headed Households, Primary Health Care, Coping Mechanism, Vulnerability
Child Headed Households[1] has recently been recognised as a new type of household structure and is a growing global dilemma (Cantwell & Holzscheiter, 2008). It has changed the household social structure from the known adult-headed to the Child-Headed Households (CHHs), the former being the key to household livelihood security. The recent notable changes in household structures have been contributed, to a large extent, by the increased number of orphans, especially double orphaned, mainly caused by pandemics such as HIV and AIDS in the 1980s, as the Ministry of Health and Social Welfare (MoHSW) (2009: p. 1; 2007a: p. 26) stated that, orphans and other vulnerable children in Tanzania have been increasing due to HIV and AIDS. Furthermore, the coronavirus Virus Disease in 2019 (COVID-19), problems such as natural calamities, wars, internal conflicts and mass migration also contributed to the increased number of orphans (Nar, 2021: p. 8).
UNAIDS (2020: p. 92) and UNICEF (2020) reported that, despite the HIV prevalence rate declining in Tanzania from 7% in 2003 to 4.6% in 2019, still the number of people living with HIV increased from 1.4 million in 2010 to 1.7 million in 2020, from which AIDS claimed deaths of 32,000 people in 2020. UNAIDS (2022) and Nar (2021) reported that with 2.2 billion children (0 – 17 years) in the world in 2021, 147 million were orphans, out of which 52 million were in Africa. Globally, of the total orphans, 15.4 million lost one or both parents due to AIDS-related complications, three-quarters of which were in Sub-Saharan Africa.
With the emergence of the COVID-19 pandemic, the death toll of people in the world has increased. U.S. Centers for Disease Control and Prevention (CDC) (2021) reported that over 175 million people were infected by COVID-19 by 2021, from which over 3.8 million people died from COVID-19-associated complications. Hillis, Unwin, and Chen (2021) estimated that close to 2 million children under 18 years old have lost one or both parents or any of their caregivers who lived in their household; of these, 1,042,000 children lost their mother or father or both. In Africa, 131,300 children were orphans by 2021 due to COVID-19.
Human migration and urbanisation transformations have also contributed to the increased CHHs, thus weakening traditional kinship systems (Foster, Makufa, Drew et al., 1997; Awino, 2010). As a result of the weakened traditional social security system and family safety nets, orphaned children were left to fend for themselves and stand alone, forgotten, and appear to be invisible to the surrounding community and the state at large (Awino, 2010; Foster, 2000; Sloth-Nielsen, 2004; Roalkvam, 2005; Rose, 2007). Furthermore, as Maclellan (2005) noted, countries experiencing conflict and warfare had witnessed a notable increase in the prevalence of child-headed households.
The 2022 National Population and Housing Census report shows that in 2022, there are 61,741,120 people in Tanzania, of which 30,257,196 (49.1%) are children under 18, with approximately 7.7% being orphans. Additionally, there are 14,297,184 households in Tanzania, from which it is estimated that 2% are CHHs (The United Republic of Tanzania (URT), Ministry of Finance and Planning, Tanzania National Bureau of Statistics and President’s Office – Finance and Planning Office of the Chief Government Statistician, Zanzibar (NBS & OCG) (2023: p. 1).
Accessing health services among CHHs has been a challenge; a study by Tsegaye (2017) revealed that 53% of children from CHHs in Uganda and 85% in Sierra Leon, medical cost was a barrier to access health services, while for those whose parents died due to AIDS-related illness, fear and stigma (Dalen, 2009; Gubwe V. Gubwe P. & Mango, 2015; Shabalala, 2013), while those who live very far from health centres cannot afford transport costs (Sibanda, 2015). In some other health centres, children not accompanied by an adult could not be attended (Sibanda, 2015; Amuge, Wabwire-Mangea, Puta et al., 2004).
The absence of economically active adults to supervise and guide children in the household opens up a new approach to life to mitigate the coming challenges; in the end, each household develops its own coping mechanisms that fit into its life pattern. Recognition of coping mechanisms is essential in understanding how children in the CHHs are faring with their livelihood security. The study was conducted in Kagera Region in Tanzania, assessing coping mechanisms applied in the CHHs seeking Primary Health Care services.
Objective
Assessing factors Influencing Coping Mechanisms in seeking Primary Health Care Services in Child-Headed Households.
Characteristics of the Study Areas
Kagera Region occupies the northwest part of Tanzania and covers an area of 40,838 square kilometres (sq.km.). Of these, 28,953 sq. km. is land, and 11,885 sq. km. is covered by water bodies. The region comprises seven administrative districts.
There are administrative Districts and Local Government Authority Councils. Seven districts have eight district councils, and Bukoba is divided into two councils: Bukoba District and Bukoba Town Council.
Biharamulo, Bukoba, Karagwe, Kyerwa, Misenyi, Muleba and Ngara. The region has 91 wards and 640 villages, with 702,412 households (NBS & OCG, Tanzania Mainland Vol. 1B, 2023: p. 16)6.
According to the 2022 National Population and Housing Census, Kagera region is the sixth most populous region in the country, with 2,989,299 people, of which 52% are children below 18. The population of the two study districts of Bukoba and Muleba is 467,386 and 637,659, of which 47.9% in Bukoba and 50.3% in Muleba are children below 18. These two districts are the most populous in the region. The region has 125,124 orphans, with 702,412 households, of which 14,048 are CHHs. (NBS & OCG, 2023: p. 170). Table 1 presents the population distribution in Kagera region.
Table 1: Population Distribution, Number of Wards, Children, Orphans, Households and CHHs by District in Kagera Region.
| No | District | # of Ward | Population | # of Children >18 | # of Orphans | # of Households | # of CHHs |
| 1.
2. |
Biharamulo | 17 | 457,114 | 267,089 | 16,292 | 87,733 | 1,755
|
| 2.
|
Bukoba | 42 | 467,386 | 223,808 | 22,605 | 122,987 | 2,460 |
| 4. | Karagwe | 23 | 385,744 | 195,839 | 13,905 | 93,366 | 1,867 |
| 5. | Kyerwa | 24 | 412,910 | 220,378 | 15,867 | 95,983 | 1,920 |
| 6. | Misenyi | 20 | 245,394 | 118,888 | 12,840 | 64,352 | 1,287 |
| 7. | Muleba | 43 | 637,659 | 320,751 | 26,622 | 149,416 | 2,988 |
| 8. | Ngara | 22 | 383,092 | 209,784 | 16,993 | 88,575 | 1,772 |
| Total Region | 191 | 2,989,299 | 1,556,537 | 125,124 | 702,412 | 14,049 | |
Source: 2022 National Population and Housing Census
Research Design And Data Collection
This study was part of a larger study assessing the effectiveness of coping mechanisms in meeting livelihood security in child-headed households in Kagera region, Tanzania. The study was characterised by a mixed-methods design in data collection, analysis and interpretation, employing both quantitative and qualitative methods. The integration of both methods, as Creswell (2014) supported, resulted in a comprehensive understanding of a problem under study rather than using a single method. In addition, other scholars (Tashakkori & Creswell, 2007; Molina & Cameron, 2010; Wiggins, 2011) added that using both methods can address and neutralise each other’s strengths and weaknesses and provide a clear understanding of research questions than using a single method. Specifically, convergent parallel mixed methods were used (Creswell & Plano-Clark, 2011). In addition, a cross-sectional design was employed; the design, as Babbie (1990) commented, allowed data collection to be done at a single point at once; also, as Casley and Lury (1987) observed, it has a greater degree of accuracy and precision in social science research. The study was sensitive and designed to fit into the emotional and social status of the children and comply with the morals and ethics. The consent of the respondents was requested before the study began.
Both qualitative and quantitative primary data were collected using a household survey questionnaire, a Focus Group Discussion (FGD) guide, a Key Informant Interview (KII), observation, and different research reports, journals, government reports, and publications.
Sample Size and Sampling Techniques
The sampling units for this study included children who headed the households, i.e., those living alone, those living with one or both grandparents and those living with and caring for a sick father or mother. These children were the family breadwinners. Both probability and non-probability sampling methods were used to develop a sampling unit.
Due to the dispersed geographic locations and heterogeneity of the population of this study, a multistage stratified random sampling technique was used to select areas for data collection. The technique was necessary as the study population was geographically dispersed with different characteristics. In this case, the government administrative system was used to select districts, wards, villages and CHHs for this study. The selection criteria were carefully crafted to ensure a diverse representation of the study area. The selection considered two key characteristics: geographical location and population demographics distribution. The geographical location was specifically focused on identifying one district with urban characteristics and another with rural characteristics. Additionally, the district’s population demographics distribution was evaluated, focusing on identifying districts with a high population, many children, and many CHHs.
Muleba and Bukoba districts were selected for this study based on these criteria. Bukoba exhibited urban characteristics, while Muleba displayed rural characteristics. Both districts also demonstrated high population numbers, a significant number of children, and a notable number of CHHs. Eight wards were selected from each district to be included in the study, ensuring a comprehensive representation of both urban and rural settings.
The participants’ sample size was calculated using Cochran’s sample size formula (Cochran, 1977). the formula states that, sample size = the population proportion (= 0.1) = acceptable sampling error (= 0.05) = value at reliability level or significance level. As Cochran (1977) elaborated, this formula allows the researcher to calculate an ideal sample size given a desired level of precision, confidence level, and the estimated proportion of the attribute present in the population. A total of 430 CHHs were included in this study, of which 45% were selected from Bukoba district and 55% from Muleba district. This distribution was reached based on each district’s percentage ratio of total CHHs. Hence, 199 CHHs from Bukoba and 231 from Muleba were included in the study. After calculating the sampling interval and choosing the 1st number randomly, every “nth” CHH was selected at regular intervals.
Data Management
The data collection tools were designed electronically to ensure data quality and minimisation of errors and the time needed for data collection, data entry, and cleaning; the data collection tools were designed electronically using KoBoToolbox. The tool is an initiative tool for collecting and producing high-quality data in challenging environments (KoBo Toolbox. (n.d.). The data collection tools were translated into the local language, Kiswahili, before the interview to ease the respondents’ understanding. Experienced enumerators were recruited to support field data collection exercises. Consideration of gender was highly observed to ensure that female respondents were interviewed by female enumerators and male enumerators interviewed male respondents. The background check was done on all recruited enumerators to ensure none had any record of violence against children or any destructive behaviours.
Recruited enumerators received a three-day training on digital data collection, safeguarding, research ethics and other issues related to research integrity and tool review. The training was conducted through two-day classroom instructions, followed by field-pre-testing exercises in both districts (covering three district councils).
Data Analysis and Interpretation
The researcher used IBM Statistical Package for Social Science (SPSS) version 25 to conduct quantitative data analysis. Microsoft Excel was also utilized for additional analysis and visualization. Primary data collected through quantitative methodologies began with a one-way tabulation of each variable to obtain the distributional features of the respondents. Then, cross-tabulations of each independent variables were done to feed their requirements.
Qualitative data analysis involved a content analysis approach, which entailed thematic exploration based on words, concepts, literary devices, and nonverbal cues by pattern matching, and exploring the interconnections among themes. Thematic procedures based on merging relevant themes and sub-themes were used to analyse data collected through FGDs, Key Informant Interviews, and observation. Responses that were similar in nature were categorized in relation to the developed themes and sub-themes, and then narratively explained in order to vividly bring out the relationship between the study variables. The exercise was preceded by data transcription. Content analysis was used to analyse data obtained from various documents. Verbatim quotations were meticulously captured in the analysis and utilized in the discussion of findings.
To control personal biases regression analysis was conducted. Further, a Chi-square (χ2) test for the significant association between objectives and variable factors that contribute to the livelihood security identified in the conceptual framework of this study and various demographic characteristics was used. Hosmer-Lemeshow goodness of fit (Hosmer and Lemeshow, 1980) was applied and all statistical inferences were made at a Confidence Interval (Cl) of 95% and a significance level of 4.73% (α=0.0473). A Pearson product moment correlation was conducted to test the relationship between variables.
Furthermore, multivariate analysis to identify associations was conducted using the logistic regression model to assess the strength or weakness of the relationship between identified variables. Erstwhile running the logistic regression analysis, the scores for the DV were recoded into two categories (i.e. dummy variables); non-affirmative responses were scored as “No” and coded 1, and the affirmative responses were scored as “Yes” and coded 0. Similarly, the dichotomous independent variables were coded into dummy continuous variables as appropriate. Thematic analysis was employed for analysis classification and exploring themes rerating to access to PHC services categories. Simple frequencies, numbers, and percentages were used to analyse data pertaining to numbers, respondent profiles, and other relevant data to obtain the proportions related to specific research questions
Ethical Consideration
The study emphasised upholding the principles of privacy, informed consent, confidentiality, and anonymity. Strict protocols were implemented to ensure that every child participating in the study received the utmost respect for their rights and best interests. Access to children was facilitated through collaboration with the social welfare departments in each district council. Furthermore, permission was sought from the village government to conduct interviews with the selected children in the sampled CHH, and a few targeted participants were engaged in FGDs at the village councils’ offices. Before the interviews and FGDs, each child’s consent was requested. Under the supervision of social welfare officers and village executive officers, informed consent was obtained through signed documents, demonstrating the researchers’ dedication to upholding confidentiality and safeguarding. Notably, despite having granted permission and signed consent forms, the respondents were apprised of their right to discontinue participation at any point during the interview.
Results
Socio-demographic Characteristics of the Respondents
The sampled population for this study was 430 respondents. The study reached all sampled respondents, equivalent to 100% of the sampled population. Female respondents were 49.5%, while male respondents were 50.5%. The distribution of the respondents per district was based on the total number of CHHs in each district and the calculation of their percentage ratio against the sampled CHHs for the study. Figure 1 shows the number and percentage of respondents reached in Muleba and Bukoba.
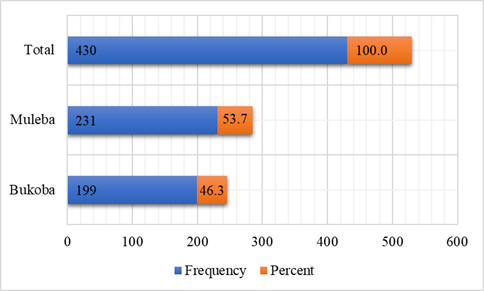
Figure 1: Respondents Reached per District (N=430)
Source: Survey Data 2023
In-depth analysis was performed to examine the socio-demographic characteristics of the sampled CHHs. The findings are summarised in Table 2, which outlines these characteristics across four key factors: the respondents’ sex, their age groups, the geographical locations of their households, and their educational attainment levels. This detailed breakdown provides valuable insights into the diversity and specific profiles of the individuals involved in the study.
Table 2: Socio-demographic Characteristics of the CHHs (N=430)
| Characteristics | Count | Percentage |
| Overall | 430 | 100 |
| Gender of the Respondents | ||
| Male | 217 | 50.5 |
| Female | 213 | 49.5 |
| Age Category of the Respondents (Years) | ||
| 7 – 10 | 35 | 8.1 |
| 11 – 14 | 238 | 55.4 |
| 15- 18 | 157 | 36.5 |
| Location /District | ||
| Muleba | 231 | 53.7 |
| Bukoba | 199 | 46.3 |
| Education Level of the Respondents | ||
| No Formal Education | 29 | 9.1 |
| Dropped out | 27 | 6.3 |
| Primary Level Education | 313 | 72.3 |
| Lower Secondary Level | 49 | 11.4 |
| High School Level | 1 | 0.2 |
| College Level | 1 | 0.2 |
Source: Survey Data 2023
In the study area, data revealed that a slight majority of households, precisely 50.5%, are led by boys, while girls head up 49.5% of these households (N=430). The analysis further highlighted that a significant majority, 55.3%, of these households are managed by children between the ages of 11 and 14, indicating that pre-adolescence to early teenage years is when many young individuals took on substantial family responsibilities. In contrast, a smaller segment of the respondents, amounting to 8.1%, comprises children aged 7 to 10, who also play a leadership role within their households.
When examining educational backgrounds, it was noted that a considerable 72.8% of the respondents had completed their primary education. However, despite achieving this educational milestone, many did not pursue further academic opportunities as they assumed the role of caregivers for their younger siblings, prioritizing family obligations over personal educational advancement. Additionally, a noteworthy 6.3% of the children had chosen to drop out of school entirely to fulfil family leadership duties, reflecting a serious trade-off between education and familial responsibilities. The average age of the respondents was found to be 14 years, illustrating that the demographic predominantly consists of early teenagers. The age range of the participants varied significantly, with the youngest being just seven years old and the oldest reaching 17, showcasing the diverse experiences of leadership among these respondents. The standard deviation in ages was calculated at 2.414, highlighting some variability in the age distribution within these caregiving roles.
Level of Vulnerability Among Children in the CHHs
It is crucial to evaluate the level of vulnerability within these households to thoroughly understand the factors that influence coping mechanisms for accessing primary healthcare services among CHHs. The study revealed that, among 430 CHH respondents, 76% lived in isolation without any adult present to provide support. In contrast, 24% indicated that an adult was either residing with them or nearby, serving in a guardian capacity.
Among the children who reported living with an adult (n=103), an overwhelming majority, 81.5%, live with their grandparents. Meanwhile, 10.7% are living with a parent who has a disability. Within this subset of children living with a parent with a disability (n=11), the findings highlighted concerning statistics: 27.2% living with mothers diagnosed with mental health conditions, while 36.4% living with mothers and fathers suffering from severe physical disabilities, which significantly impacted their ability to care for their children.
Despite the presence of an adult in these households, many were either too aged or gravely ill to fulfil parental roles effectively. As a result, these children often found themselves in a position of responsibility, forced to assume the role of head of the household. This shift in roles placed immense pressure on them. It compelled them to take on the burden of providing for the household’s basic needs, navigating the complexities of daily life in a challenging environment.
During the study, it was observed that children living in those households faced several challenges, such as a lack of parental care, affection, and emotional support. This exacerbates their feelings of neglect and exclusion, significantly impacting their overall well-being. Merely 7.7% of CHHs in Bukoba and Muleba districts (N=430) reported the presence of close relatives living close by, while 65.5% acknowledged the existence of other relatives residing elsewhere in the country. Given the significance of familial connections, examining the frequency of visits made by these relatives to the children residing in CHHs was imperative. Regular visits from family members play a crucial role in nurturing and fortifying the familial bond, fostering a sense of love and acceptance, providing child-centred support, and upholding close-knit family ties. Figure 2 illustrates the frequency of relatives’ visits to the CHHs.
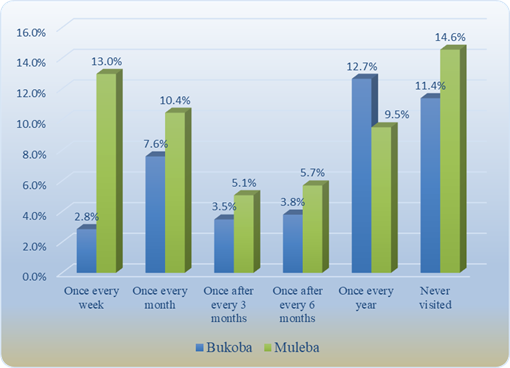
Figure 2: Frequencies of Relative Visits by District
Source: Survey Data 2023
Although most CHHs have relatives residing either in close proximity or elsewhere within the country (n=315), it was observed that only a small fraction, 15.8% received visits from their relatives at least once a week. Additionally, 22.2% were visited at least once per year, while a concerning 26% reported that they had never been visited by their relatives at all, highlighting a notable disconnect in familial relationships despite geographic proximity.
Access to the Primary Health Care Services
Access to health care has been defined by the Institute of Medicine (IOM) (1993, p. 4) as “the timely use of personal health services to achieve the best health outcomes”. The author further emphasised that to assess whether access to healthcare has been effectively attained, it is crucial to observe both the utilisation of health services and the resulting health outcomes. Timely use can be categorised as the ability to access services when needed. Levesque, Harris, and Russell (2013) further elaborated that accessibility can be categorised into five dimensions: Availability, Acceptability, Approachability, Affordability, and Appropriateness.
This study assessed the availability and geographical aspects of health services. It was found that 56.7% of the respondents (N=430) declared that health services were available nearby in their areas of residence. For those who responded that health services were available, the study explored accessibility by looking at the distance to the health service from their households. Figure 3 shows the distance from home to the health facilities.
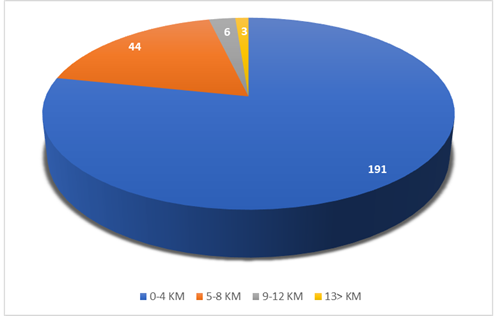
Figure 3: Distance from Home to the Health Facilities (N=244)
Source: Survey Data 2023
On average, the distance from the CHHs to the nearest health facility is approximately 2.8 kilometres. The closest health facility is situated just 1 kilometre away, while the farthest one extends to a considerable distance of 16 kilometres. The study uncovered a striking reality. Despite the alarming rate of sickness among children residing in the CHHs, an astonishing 64.9% of the respondents disclosed that they had not sought medical attention at health facilities over the past year. Even though a significant number of CHHs, are situated in close proximity to essential healthcare facilities, the study found the level of accessibility to these services remains alarmingly low. This finding indicates that there are likely numerous barriers at play beyond just the geographical distance. Potential factors could include socioeconomic challenges, lack of transportation options, and insufficient awareness about available services, all of which could prevent individuals from readily accessing the healthcare they require. Such insights highlight the complexity of healthcare accessibility and suggest that a more comprehensive understanding of these obstacles is essential for improving service utilization in the community.
Furthermore, the study explored the association as to why there is a considerable group of CHHs who do not attend the health facilities, whereby a logistic regression was conducted to assess the strength of the relationship between health facility visits when felt sick (as a dependent variable) versus gender, age, living arrangement, distance from home as well as education level as independent variables. Horsmer-Lemeshow goodness-of-fit was applied with the odd ratio of 95 per cent (CI = 95%). Prior to running the logistic regression analysis, the scores for the Dependent Variable (DV) were recoded into two categories (i.e. dummy variables); non-affirmative responses were scored as “No” and coded 0, and the affirmative responses were scored as “Yes” and coded 1. Similarly, the dichotomous independent variables (gender, age, living arrangement distance from home and education level) were recoded into two values and coded as either 0 or 1. Table 3 shows further analysis of the strength of the relationship between health facility visits when sick versus gender, age, living arrangements, distance from home, and education level.
Table 2: Relationship Between Health Facility Visits Versus Gender, Age, Living Arrangements, Distance from Home, Education Level of the Respondents (n=222)
| B | S.E. | Wald | df | Sig. | Exp(B) | 95% C.I. for EXP(B) | |||
| Lower | Upper | ||||||||
| Step 1a | Gender of the respondents | -.178 | .284 | .392 | 1 | .531 | .837 | .479 | 1.461 |
| Age of the respondents | -.139 | .066 | 4.364 | 1 | .037 | .871 | .764 | .991 | |
| District | -.318 | .290 | 1.205 | 1 | .272 | .728 | .413 | 1.284 | |
| Living Arrangement | .080 | .322 | .061 | 1 | .804 | 1.083 | .576 | 2.035 | |
| Distance to the PHC facilities | .098 | .054 | 3.316 | 1 | .069 | 1.103 | .993 | 1.226 | |
| The level of education of the respondents | .101 | .435 | .054 | 1 | .817 | 1.106 | .471 | 2.596 | |
| Constant | 2.521 | 1.205 | 4.373 | 1 | .037 | 12.437 | |||
Source: Survey Data 2023
A total of 222 CHHs were analysed, and from the findings, it was observed that;
The odds of the CHH members who live with an adult at the household attending health facility were 1.083 times higher than those who live with no adult in their household, with a 95% CI of .576 to 2.035
The odds of the CHH members attending a health facility when the facility is near their home were 1.103 times higher than those whose distance from home to facility is longer, with a 95% CI of .993 to 1.226
Again, the odds of the CHH members who have higher levels of education attending health facilities were 1.106 times higher than those with lower levels or no education at all, with a 95% CI of .471 to 2.596
Other factors (gender, age, and location) do not likely contribute to the occurrence of the event (attendance at the health facility when feeling sick).
Looking at the affordability, in Tanzania, access to health services is contingent upon having insurance, qualifying for exemption or being waived. The provision of free health services changed in the early 1990s when Tanzania enacted a user-fee policy (cost-sharing) in 1993 (MoHSW, 2007b). in that sense, individuals must pay in cash when visiting the PHC facilities. The study found that 35.1% of respondents (N=430) sought health care services when a household member felt ill. Among those who managed to visit the facilities (n=151), the findings revealed that 68.2% paid for the services, while only 30.4% received a waiver and received free services. A thorough investigation was conducted to ascertain how the expenses were managed among those paid for the services and the sources from which the funds were obtained to cover the costs of the services rendered. Figure 4 illustrates sources of funding to cover health expenses presented by percentage and by district.
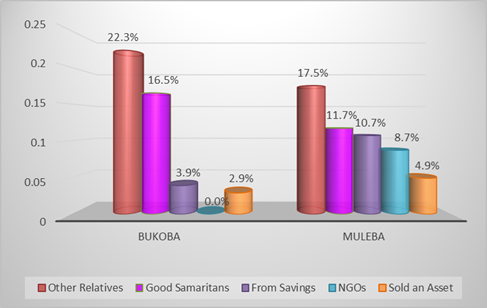
Figure 4: Disaggregation of the Source of Money in the CHHs to Cover Health Services Expenses by District (n=103)
Source: Survey Data 2023
Among those who visited the facilities and made cash payments for Medicare services (n=103), it was observed that 39.8% depended on financial assistance from their relatives as their primary means of covering health-related expenses. Additionally, 28.2% of the children living in CHHs within Muleba and Bukoba districts received aid from good Samaritans. In challenging circumstances, some children in CHHs resorted to liquidating their assets to finance their medical expenses, with 4.9% in Muleba and 2.9% in Bukoba district adopting this strategy. This strategy was also reported by Gow, Desmond and Ewing (2002) that evidence from Tanzania and Uganda showed that there was an increase in radio ownership in the households with no nay deaths while there was a decrease in the households that experienced parental death. Notably, the findings indicated a complete absence of government support in the study area.
A closer examination of the accessibility of health services, combined with insights garnered from the Focus Group Discussions (FGDs), reveals that children residing in CHHs face a myriad of significant obstacles when attempting to access healthcare. These hurdles manifest in various forms, such as a pervasive lack of respect from healthcare providers, which can discourage these children from seeking help. Many also experience inadequate access to essential medical services, which is compounded by overt harassment, bullying, and discrimination at the hands of health workers.
These negative experiences are often intensified by practical barriers, including their inability to pay for medical services and the lack of health insurance cards, which can prevent them from receiving necessary treatment. Additionally, the absence of an adult to accompany them during visits to health facilities often leaves these children feeling vulnerable and unsupported. Consequently, due to these compounded factors, disrespect, financial constraints, and social stigma, many children from CHHs tend to avoid visiting PHC facilities altogether when they are feeling unwell, further compromising their health and wellbeing.
Copying Mechanisms Applied in Seeking Primary Health Care Services
The alteration in family structures necessitated that children left behind establish new family frameworks, resulting in alternative arrangements for their survival. The study found that some children voluntarily chose to reside in the CHHs in order to safeguard the property left by their parents. Whether by choice or circumstance, children living in these households demonstrated an awareness of the challenges they would encounter. Although the adaptation process proved demanding, they exhibited resilience in the face of difficulties in accessing primary healthcare services, managing associated costs, and coping with limited availability resulting from geographic distance. Households unable to cover medical expenses or secure a waiver developed tailored coping strategies to meet their primary healthcare needs when unwell. Figure 6 illustrates the various mechanisms CHHs employ to address health-related challenges effectively.
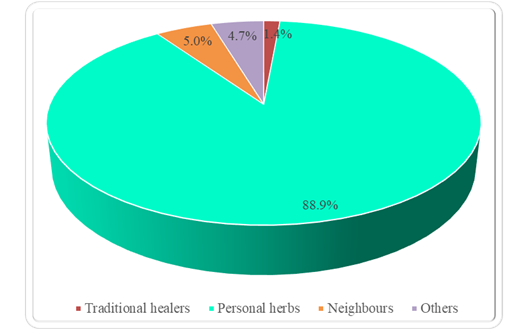
Figure 6: Coping Mechanisms Used in the CHHs to Mitigate Health Problem (n=279)
Source: Survey Data 2023
The research revealed that an overwhelming 88.9% of individuals who did not visit health facilities (n=279) relied instead on personal, unprescribed herbal remedies for self-treatment. Among these cases, a noteworthy observation was that nearly half (47%) of children residing in the CHHs within Muleba district reported opting for personal herbs as their method of self-care. This figure contrasts with the 42% of children in Bukoba district who similarly turned to herbal self-treatment. Furthermore, a small segment of the population, about 5%, indicated that they procured medicines from neighbours, while a mere 1.4% sought guidance from traditional healers. These statistics highlight the prevalent use of herbal remedies and the limited engagement with formal medical services in the CHHs.
Factors Influencing Copying Mechanisms in Seeking Primary Health Care
The study considered the lack of knowledge on the availability of health services exemption and waiver policy for vulnerable people as among the factors that limit children in CHHs’ access to health services, hence influencing the creation of other coping mechanisms to mitigate health problems.
The study revealed a concerningly low level of awareness among households about the policy designed to exempt and waive fees for health services specifically for vulnerable groups. Out of a total of 430 respondents, a significant 77.9% are unaware of this important policy. This lack of awareness is particularly striking in Bukoba district, which serves as both the major urban centre and the capital of the region; here, only 7.7% of CHHs reported being informed about the health services exemption and waiver policy. In comparison, awareness was slightly higher in Muleba district, where 14.4% of the households recognized the policy’s existence.
Overall, only 22.1% of the CHHs across the study area acknowledged any knowledge of the exemption and waiver policy intended for vulnerable populations. Among this group of knowledgeable participants, which consisted of 95 individuals, only 63.2% indicated that some of their family members living in the CHHs had actually benefited from the waiver, allowing them access to Medicare services without the burden of payment. These finding highlights both the gaps in knowledge about essential health policies and the limited real-world impact these policies have had on the targeted vulnerable groups.
Surprisingly, the findings also revealed that government officials, specifically social welfare officers and health workers, do not understand the health service exemption and waiver policy for vulnerable groups and how it should be executed. There is a mixed definition and understanding of the applicability of the policy. During the Key Informative Interviews (KIIs) with the social welfare officers, they revealed some confusing information concerning the understanding of the exemption and waiver policy. Some noted that children from marginalised or highly vulnerable demographics receive an exemption during the first five years of life. Following this period, exemptions are not granted unless the child has a chronic illness or disability. Conversely, others indicate that the practice of granting exemptions is primarily extended to individuals living with HIV.
The chi-square test was analysed to confirm any relationship between children living in the CHH health facility visit and the knowledge of the existence of health policy exemption and waiver for vulnerable people. From the findings, it was noted that there is a statistically significant association between CHH health facility visits and the knowledge of the existence of health service exemption and waiver policy for vulnerable people, as a chi-square test of (x2=10.592, df=1, p=.001) was observed. Therefore, the study concludes that knowledge of the existence of exemption and waiver policies for vulnerable people is an associating factor for CHHs’ attendance to the health facility when they feel unwell, without which other coping mechanisms will be developed to mitigate health challenges in the household.
Furthermore, logistic regression was conducted to test if household size, education level, age of the youngest person in the household, gender of the head of the household, and distance to the health facility from home, as well as the age of the head of the household, were associating factors for CHHs to visit or not to visit health facility when felt sick. Horsmer-Lemeshow goodness-of-fit was applied with the odd ratio of ninety-five per cent (CI = 95%).
The overall accuracy rate of the study was impressive, standing at 66.9%. This outcome indicates a strong level of precision in the predictions made. Notably, the results reflect commendable sensitivity, as 72.3% of the respondents who reported not visiting healthcare facilities when they experienced illness were accurately anticipated to avoid seeking medical care during times of sickness. This suggests that the predictive model effectively captures the behaviour of individuals who refrain from utilizing health services, highlighting its reliability in identifying those less likely to seek treatment under such circumstances.
A total of 279 CHHs who responded not to attend health facilities when they felt sick were analysed, and from the findings, it was noted that;
The odds of the CHHs who do not attend health facility when feeling sick is 1.200 times higher for those with low level/no education as compared to those with high level of education, with a 95% CI of .869 to 1.658
The odds of the CHHs who do not attend health facility when feeling sick is 1.002 times higher for those who have siblings with lower age as compared to those with siblings with older ages, with a 95% CI of .887 to 1.132
The odds of CHHs who do not attend health facilities when feeling sick are 1.214 times higher for BHHs than GHHs, with a 95% confidence interval of .525 to 2.811.
The odds of CHHs not attending health facilities when feeling sick are 1.238 times higher for respondents whose households were far from the health facility than those closer to the health facility, with a 95% confidence interval (CI) of 1.050 to 1.459.
The odds of CHH members who live with adults in their households attending health facilities when they feel sick were 1.515 times higher than those who live alone, with a 95% confidence interval (CI) of .528 to 4.346.
The odds of CHH members attending health facilities for CHHs with less than a few years as head of the household were 1.261 times higher than those who have been the heads of the household for more years, with a 95% confidence interval (CI) of 1.022 to 1.556.
The size of the household and the age of the head of the household has no significant association with visits to health facilities when one feels sick.
Therefore, the findings conclude that education level, age of siblings, gender of the head of the household, the distance to the health facility, and the number of years the head of CHHs has been heading the household were the associating factors that influenced children living in the CHHs to visit or not to visit the health facility when they felt sick.
With no government support for CHHs to access healthcare services and the absence of a dedicated budget or initiatives to support CHHs when they feel sick, less or no knowledge of the health service exemption and waiver policy among vulnerable groups has been a challenge to their access.
The essence of this study was triggered by the resilience demonstrated by children in CHHs. The need to assess the effectiveness of coping mechanisms applied in those households was vital to see its contribution to their well-being. Poor or no access to PHC services affects their well-being and academic performance. Some of the CHHs were found to be still supported by their existing relatives, others by Good Samaritans, while the majority are engaged in working as labourers in farms, fisher’s landing beaches and bricks-making sites. Tragically, a significant number resort to begging on the streets, many of whom come from girl-headed households (GHHs) where the quest for survival has turned to financial desperation. Despite being a lifeline to offset medical expenses, the involvement of children, particularly girls, in these laborious efforts exposes them to heightened risks and vulnerabilities, including the risk of exploitation and sexual abuse.
The inadequate social welfare systems significantly hinder the well-being of children living in CHHs, aggravated by insufficient enforcement of existing child protection and safeguarding frameworks and the minimal assistance offered by government agencies. This failure to provide robust support creates a cycle of vulnerability for these children. According to a report by the Ministry of Health and Social Welfare, the actual needs of the country’s vulnerable population, particularly those in precarious situations like CHHs, have not been fully mapped and addressed (MoHSW, 2009, p. 39). This gap leaves many children without the necessary resources and protections, further entrenching them in a state of instability. Their access to essential health services remains worryingly out of reach. Moreover, the findings indicate that these children are often grouped under the umbrella of Most Vulnerable Children (MVC). This classification includes those who may not be in immediate need but face significant hardships. This oversight results in the sweeping generalisation of CHHs as mere representatives of the MVC, a categorisation often linked to the devastating impact of AIDS, despite the reality that not all CHHs have arisen from such circumstances.
In 1990, Tanzania established the Ministry of Community Development, Gender, and Children (MoCDGC) to safeguard and uphold children’s rights nationwide. However, amidst the persisting hardships faced by CHHs, questions loom regarding the effectiveness of this ministry in fulfilling its mandate to protect and nurture these vulnerable children. The existing gap between the directives outlined in policy frameworks and the harsh realities experienced in CHHs underscores the inadequacy of supportive measures within the MoCDGC. CHHs remain invisible, failing to gain recognition as legitimate household models in Tanzania. Instead, prevailing legal structures continue to uphold the notion that only parents and guardians can serve as household heads.
The growing trend of covering medical expenses significantly exacerbates the financial strain on children who head the CHHs. In these situations, the absence of adult caregivers places an extraordinary financial burden on the young heads of these households, making them more susceptible to various vulnerabilities. These children often struggle to manage the costs associated with routine healthcare and the unexpected medical emergencies that can arise. As a result, their ability to afford necessary treatments is compromised, further increasing their risk of suffering from health-related issues, which can create a cycle of poverty and instability within these already fragile family structures.
The research revealed that many respondents in CHHs within the study area refrained from seeking medical attention at healthcare facilities. This growing trend is concerning and seriously risks their overall health and well-being. The implications of this situation are alarming, as the absence of timely medical care can lead to the deterioration of health conditions that could otherwise be managed or treated effectively. The focus group discussions provided valuable insights into the difficulties many children living in CHHs face when they seek medical care at health facilities. These children often endure a range of complexities that obstruct their access to essential health services. One prominent issue is the disrespect they frequently encounter from healthcare workers, which can manifest as a lack of empathy and support. Additionally, many children reported instances of being denied services altogether, leaving them without crucial medical assistance.
Beyond these interpersonal challenges, the children recounted experiences of harassment, bullying, and discrimination within healthcare settings, all of which contributed to an environment of hostility and discomfort during their visits. This negative atmosphere can prevent children from seeking health care when they need it most. Further compounding these issues are financial barriers. Many children do not have sufficient cash to pay for medical services at the point of use, which is often exacerbated by the absence of proof to be insured that could otherwise mitigate these costs. Additionally, some children find themselves denied access to health services without an adult companion during their visits, which amplifies their feelings of vulnerability and isolation, making the already daunting experience of seeking healthcare even more challenging. Evidently, the attitudes of health service providers, personal characteristics, misconceptions about the age requirement for unaccompanied minors, and a lack of knowledge about the legal framework impact the health-seeking behaviour of children living in CHHs.
The study reveals a significant gap in providing free primary healthcare services for children residing in CHHs. Many of these households encounter numerous obstacles when attempting to access quality health services at public health facilities. Following the introduction of a cost-sharing policy (user fees) for healthcare services in 1993, which aimed to improve efficiency and foster sustainability in the provision of health services in Tanzania through the participation of community members, the government identified significant barriers to accessing healthcare for the country’s poor and vulnerable populations (MoH, n.d). To promote equitable access to primary healthcare services, the Ministry of Health introduced an exemptions and waivers policy in 1994. This policy aimed to ensure that vulnerable groups within society could access vital health services without financial obstruction.
Under this framework, exemptions were identified as statutory entitlements automatically granted to specific vulnerable groups. These groups include pregnant women, children under five years of age, and individuals suffering from certain devastating chronic diseases, such as tuberculosis (TB), leprosy, cancer, and HIV and AIDS, which place a heavy financial burden on affected families (MoH, 2003, p. 28). Conversely, waivers were designed for those in dreadful economic situations who could not afford to pay for healthcare services. To qualify for these free services, individuals must undergo the waiver processes outlined in the National Cost-Sharing Guidelines and Community Health Fund: Operational Guideline (MoH, n.d., p. 14). The individuals should demonstrate their inability to pay due to their socioeconomic status.
In 1999, the policy was expanded to include elderly individuals aged 60 and above, recognising their distinct needs and vulnerabilities. These initiatives aim to prevent the exclusion of marginalised groups and foster more significant equity in healthcare access across the nation. However, the policy’s definition of ‘vulnerable populations’ is relatively narrow and does not explicitly address the needs of children living in CHHs. Children over the age of five within these households must also undergo the waiver process, rather than being exempted, which is contingent upon the subjective judgment of local village leaders and a designated committee assessing their eligibility for waiver assistance.
Despite these efforts, the exemption and waiver systems have largely fallen short of their intended purpose. This shortfall can be attributed to a widespread lack of awareness and relevant policy information among community members and certain government officials, particularly health and social welfare workers. Thiede, Akweongo, and McIntyre (2007) noted that adequate access to PHC services is intrinsically linked to disseminating clear and comprehensive information. The failure to implement the exemption and waiver policies actively and efficiently has inadvertently marginalised the very vulnerable demographic of CHHs, depriving them of necessary health services. This exclusion is contributed by the lack of proper dissemination of information, education and communication, a sentiment echoed by the Ministry of Health (2005), along with various researchers, Mliga, Mwakilasa and Mwakalukwa (2005), and Kiwara, Mujinja, and Chitama (2005), who highlight the critical need for better communication and education regarding healthcare access entitlements.
The study findings revealed that most CHH children are mainly unaware of the existence and benefits of this health exemption and waiver policy. Furthermore, health and social welfare workers often misinterpret these guidelines, leading to confusion and misinformation that significantly obstructs these children’s access to essential PHC services. The uncertainty surrounding the health exemption and waiver policy has serious implications. This lack of clarity not only diminishes the support available to children in CHHs but also effectively denies them their right to receive free healthcare. Consequently, these young individuals, who are already in precarious living situations, are left without the necessary medical care that could enhance their overall well-being and quality of life.
Managing a household at a younger age is stressful for both the head of the household and the siblings living in that household. Stress encountered by CHHs in seeking PHC services leads to the development of various coping mechanisms to mitigate the needs of PHC. The findings corroborated by the research of Lazarus and Folkman (1984) establish that their cognitive Theory of Coping suggests individuals do not merely acquire new behaviours through trial and error; rather, they employ specific coping strategies as critical mechanisms for survival. Additionally, Stanisławski (2019), Frydenberg and Lewis (1993), and Gol and Cook (2004) indicate that stress or stressful conditions act as catalysts for the development of coping mechanisms at both individual and household levels.
Psychologists Richard Lazarus and Susan Folkman also advocated this situation in 1984, when they developed the Transaction Theory of Stress and Coping, along with the Coping Circumplex Model introduced by Stanisławski (2019). Both theories present a comprehensive understanding of how individuals respond to stress and adapt their coping mechanisms. Both theoretical frameworks emphasise the pivotal role of stress as a central element influencing the effectiveness and choice of coping strategies.
In this context, coping is understood as a complex process that individuals engage in when faced with stressful situations. The theories highlight two primary coping strategies: problem-focused coping and emotion-focused coping. Problem-focused coping involves taking proactive steps to address the source of stress through practical solutions and actions, thereby reducing the stressor itself. This approach is particularly effective when the individual believes that they can change or manage the environmental factors contributing to their stress.
Conversely, emotion-focused coping is centred on managing the emotional responses that arise from stressors rather than attempting to change the situation itself. This strategy may include methods such as seeking social support, engaging in relaxation techniques, or reframing the situation to alter its emotional impact. Both models provide valuable insights into how stress influences coping behaviour, ultimately guiding individuals toward more adaptive adjustment mechanisms in the face of life’s challenges.
The research findings thoroughly explored the coping mechanisms in health-seeking behaviours exhibited by children living in CHHs in Bukoba and Muleba districts. The study revealed that a substantial majority apply problem-focused coping to solve challenges related to health accessibility. The majority turn to traditional herbal remedies as their primary coping method of self-treatment when confronted with health issues. This reliance on herbal remedies signifies a deep-rooted cultural connection to conventional healing practices learned from their parents. However, it is highly contributed by the challenges CHHs face to access PHC services. Other children also seek assistance from local traditional healers who operate within their villages or nearby neighbourhoods. These healers often use a combination of local knowledge and natural resources to address their health concerns.
The preference for these coping mechanisms stems from various factors, including limited financial resources and a lack of information about the existing health services exemption among vulnerable populations. Additionally, the exemption policy is translated differently among government officials, which leads to poor enforcement. Hence, the right to exemptions from paying medical expenses is systematically denied, further restricting their choices and undermining their autonomy in making informed health decisions. This situation calls for an urgent need for targeted interventions to improve access to healthcare while educating CHHs and social and health workers about the existing exemption policy.
Tanzania Health System Overview
Tanzania’s health system is structured hierarchically, reflecting the administrative organization of local governance. At the foundational level, health services begin with dispensaries located in villages. These are complemented by health centres at the ward level and district hospitals at the district level. At the regional level, regional referral hospitals are established, further supplemented by zonal hospitals, culminating in the national hospital at the apex of the system. Certain specialized hospitals integrate directly into this hierarchy and maintain a direct link with the Ministry of Health.
The Tanzanian government has implemented several strategic plans and policies aimed at guiding healthcare provision and development to ensure comprehensive primary healthcare access for all citizens. The first national health policy was instituted in 1990 and remained in effect until a revision in 2007, with a renewed focus on promoting healthy communities as a foundation for national development. The 2017 revision introduced the third National Health Policy, which articulates the goal “to reach all households with essential health services that meet population needs, adhere to quality standards, and apply evidence-informed interventions through resilient health systems” (Ministry of Health, Community Development, Gender, Elderly and Children {MoHCDGEC}, 2017, p. 38).
This policy framework emphasizes gender equity and equal access to health services. A core commitment is to prioritize equitable service provision, particularly for vulnerable populations residing in remote areas and impoverished district councils (MoHCDGEC, 2017, p. 38). However, the policy lacks specificity in defining the extent of vulnerability and fails to adequately address the needs of children living in CHHs, as noted by MoHSW (2009), indicating that the actual conditions and risks faced by vulnerable groups remain poorly mapped and recognized.
The organization and financing of the health system are critical determinants of overall health outcomes. Since the early 1990s, health financing has emerged as a pivotal issue as the government seeks to enhance systemic healthcare. The unsustainability of providing universally free health care became apparent due to rising healthcare costs and economic strains. Consequently, health sector reforms initiated in the early 1990s transitioned from a purely free service model to a mixed financing approach that incorporated cost-sharing mechanisms (MoHSW, 2007b).
The Health Sector Reform (HSR), launched in 1994, aimed explicitly at enhancing access, quality, and efficiency of healthcare delivery. Subsequently, in 2009, the Health Sector Strategic Plan (HSSP III) was initiated (MoHSW, 2009). Despite these advancements, the current financing frameworks lack adequate social protection, heavily relying on out-of-pocket expenditures, thus imposing severe and sometimes catastrophic financial burdens on disadvantaged households, including those led by children, thereby hindering equal and sustainable access to essential healthcare services.
The Exemption and Waiver Policy, integral to the cost-sharing framework introduced in 1994, intends to facilitate access to quality health services without financial hardship for specified beneficiaries. Eligibility for exemptions from user fees at primary care facilities is conditioned upon chronic or epidemic diseases, pregnancy, children under five, and individuals aged 60 and older. Additionally, waivers can be granted to the poor, vulnerable individuals, and those affected by emergencies, this category encompasses disabled persons, orphans, street children under 18, those struggling with substance use, and victims of war or natural disasters. Despite the policy’s intentions, numerous institutional and behavioural challenges have impeded its effective implementation since its inception.
A robust primary healthcare system serves as the entry point for the majority of the population into the healthcare landscape. Acknowledging the challenges of equitable healthcare access across geographical boundaries, the Community Health Fund (CHF) was introduced in 2001 with the intention of achieving universal health coverage. In 2021, the MoHCDGEC unveiled the fifth Health Sector Strategic Plan (HSSP-V) for 2021-2026. This strategic blueprint emphasizes vulnerable populations and seeks to enhance equity in the provision and accessibility of primary healthcare services, focusing on four strategic pillars.
Despite all these efforts, there are still gaps in addressing the PHC needs of orphans, specifically of the children living in CHHs. The magnitude of their health needs is not yet well recognised by the government and other stakeholders supporting them. MoHSW (2009) indicated that there is less collaboration between health and social welfare officers, and the health needs of orphans have been combined in the HIV and AIDS interventions under the umbrella of care and support, forgetting that AIDS does not necessarily cause orphan-hood.
Conclusion
The existence of CHHs in our communities reveals a troubling fracture within the fabric of the extended family system. As traditional household structures evolve, orphaned children find themselves navigating a harsh reality where they must seek out alternative living arrangements. In the face of adversity, these resilient young individuals have resourcefully crafted various coping mechanisms, striving to secure sustainable livelihoods. They confront numerous risks and vulnerabilities tied to their unexpected roles as household leaders, demonstrating remarkable strength and adaptability at such tender ages.
The transformation of Tanzania’s health system over the last three decades is evident in the government’s good intention to provide equity in health service provision. However, our legislative systems still do not recognise CHHs as a family unit; instead, they are blanketed under the Most Vulnerable Children space while children in the CHHs care for themselves to attain their livelihood. A child heading the household is tasked with making day-to-day decisions on the welfare of siblings living in that household. However, they encounter age barrier vulnerability when accessing PHC services since they were not accompanied by an adult to PHC clinics.
The analysis revealed significant shortcomings in the implementation of the exemption and waiver policy, which critically impaired access to quality health services for children living in CHHs. These children faced not only barriers to obtaining necessary medical care but also experienced social stigma and disadvantages when compared to patients who could afford to pay for services. This discrepancy highlighted a troubling potential conflict of interest, where health facilities prioritized revenue generation over the protective objectives of the policy designed to aid the most vulnerable populations.
Access to PHC services is a stipulated human right, with no exception for children living in the CHHs. However, ignorance of policy frameworks and guidelines among the social welfare and health workers on the existence of health exemption and waiver policies to the children living in the CHHs create barriers to enjoying the rights given to those children, mistreatment by the health service providers and hostility of health service providers, lead to the adaptation of the coping mechanisms at the expenses of their well-being by jeopardising their life by using unprescribed medicines.
Furthermore, it was evident that health facilities lacked sufficient motivation to grant exemptions from user fees. The absence of a reimbursement mechanism meant that these institutions could not recover the costs associated with providing care to exempted patients. As a result, those who were actually eligible for support under the policy often found themselves unable to access affordable healthcare. This situation necessitates a thorough reassessment of both the policy implementation framework and the incentives within health facilities to ensure equitable health access for all children in need.
Recommendations
In light of these findings, the study puts forth several recommendations designed to stimulate further research, call for the review of existing policies, strategies, and regulations, as well as to strengthen the support systems implemented by both government agencies and non-governmental organizations. These recommendations aim to foster a more effective framework to assist these resilient children in their journey toward sustainable livelihood security.
Declaration of Conflict of Interest
The author affirms that this study was independently funded; therefore, no identified financial interests or personal relationships may have influenced the findings presented in this paper. Therefore, the author declares that there is no conflict of interest to disclose.
Ethical Approval
The researcher completed all mandatory requirements to obtain the research permit. Ethical clearance was obtained from the Vice Chancellor of the University of Dar es Salaam (see attachment I).
Data availability
This study involves participants who are individuals under the age of eighteen. Given the sensitive nature of research concerning children, the data collected are not available for public dissemination as they contain information that could jeopardize the privacy of the research participants. Nonetheless, for verification purposes, access to this data may be requested from the corresponding author, Dr. Florian Silangwa.
Consent to participate
Strict protocols were followed to ensure that all children participating in the study were treated with utmost respect for their rights and best interests. Each participant signed informed consent under the supervision of Social Welfare Officers.
This study defines a child-headed household as one managed by a child (8 – 17 years old) who has lost one or both parents or is living with an elderly relative (60 years and above) or chronically ill parent. The child takes on the responsibility of heading the family and being the breadwinner for the whole family (author’s definition, 2019).